Organ prolapse — have you heard of it? Did you know that most mamas are unaware they even have it? In a very informative interview, Kelly of Priority PT is breaking down everything about organ prolapse, how physical therapy can help, along with resources that will lead you to a positive outcome. See what Kelly has to say below!

What is organ prolapse?
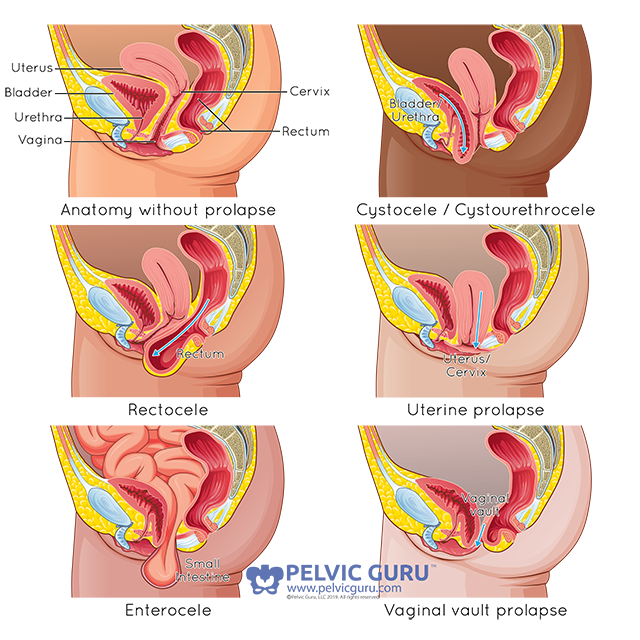
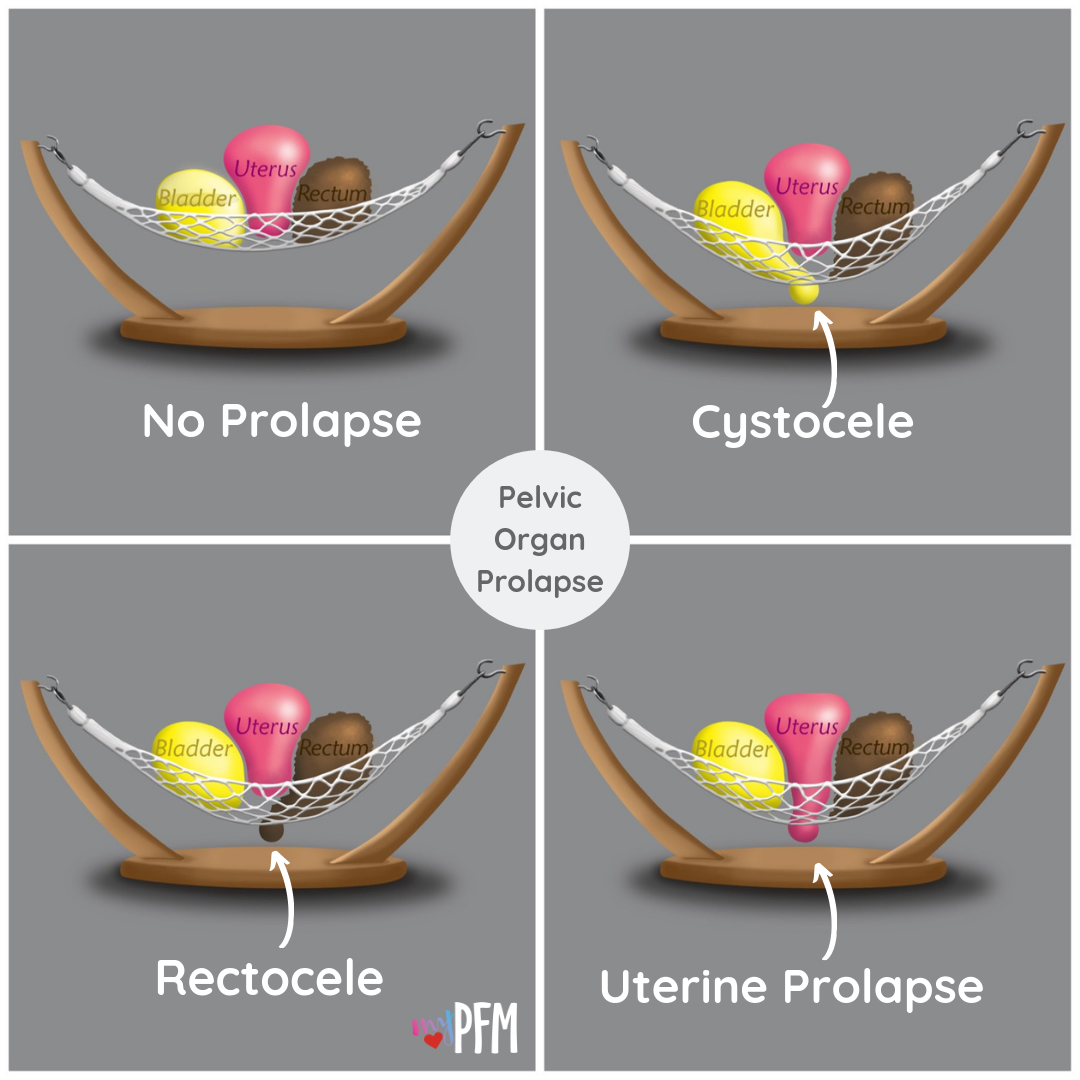
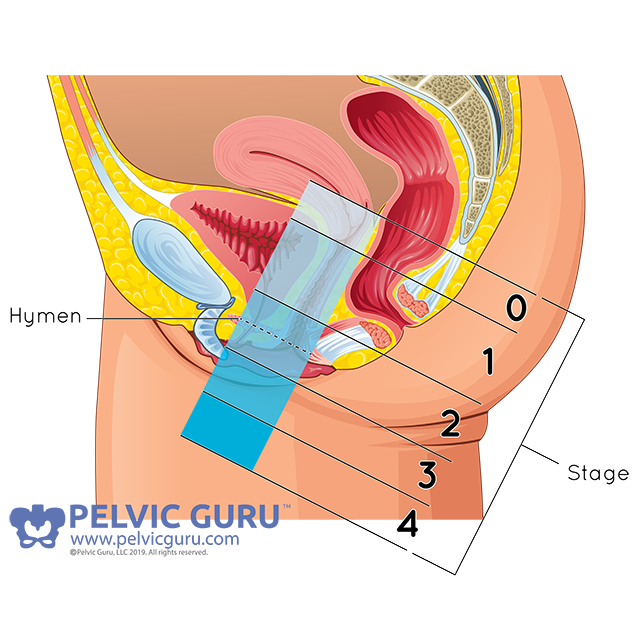
Kelly: Pelvic Organ Prolapse (or known as POP) is when the organs within your pelvis start to shift down into the vaginal canal. There are several different kinds of prolapse and they can involve the different structures in the pelvis: the anterior wall with the bladder known as a cystocele, the posterior wall with the rectum known as a rectocele and/or the apex where the the uterus and cervix are located. Some women may have a combination, but these are among the most commonly seen diagnoses. We classify the severity of prolapse based on the amount of descent into the canal from first state to fourth stage (generally doctors will diagnose but a physical therapist can screen to let you know which side is affected). The states are based on where the organ is in relation to the vaginal opening or hymen at rest and where the organ tends to rest or be pushed down with regard to internal pressures changing. Sometimes standing is better to assess than lying down just based on gravity and real life so if you notice something when you are jumping or after activities, you should assess after those activities are performed to get a true assessment of your baseline.
Why should mamas get this checked out?
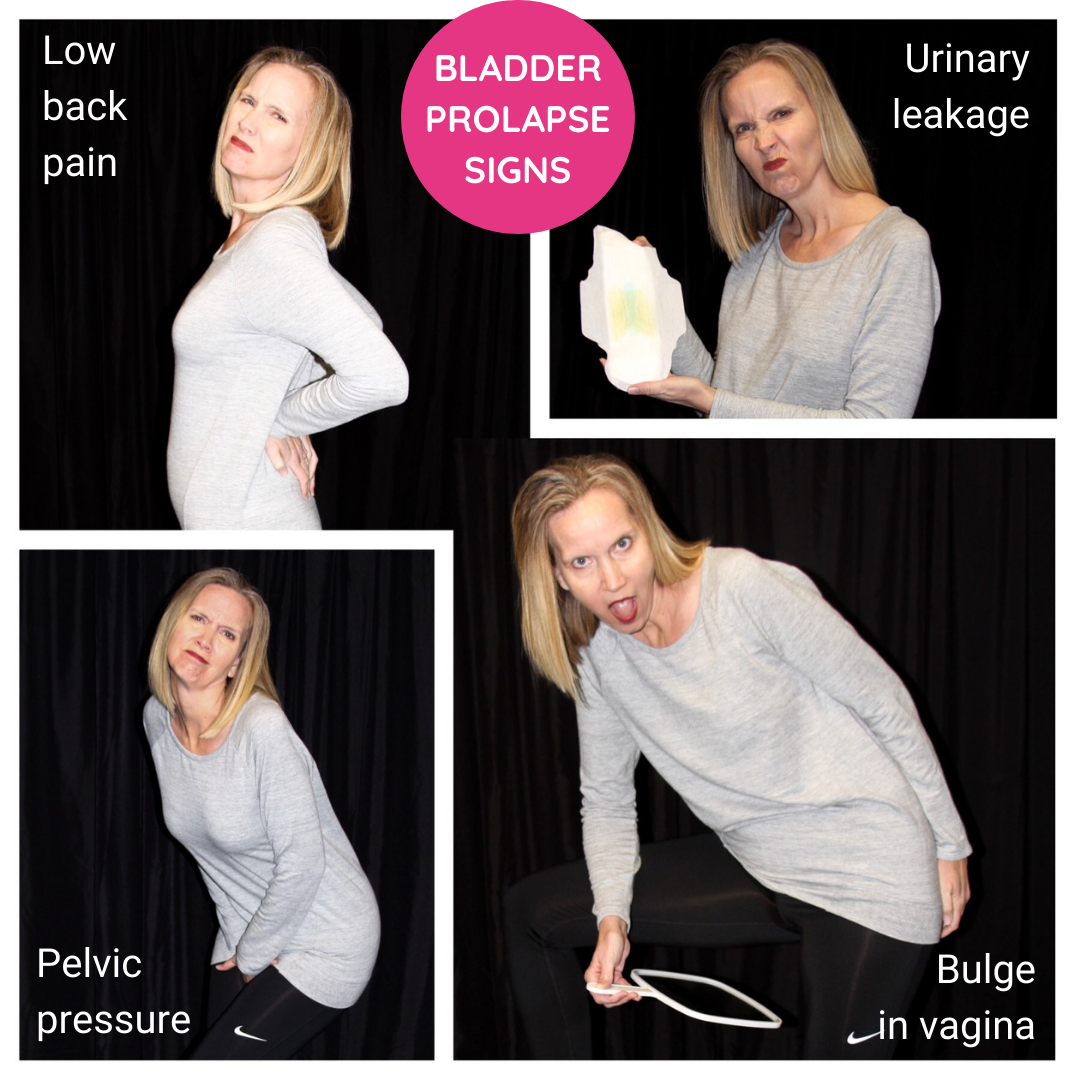
Kelly: Mamas should get checked to have a baseline for their own body. If we look at the statistics, at least 50% of us have a prolapse despite not “feeling” something different. It’s beneficial for us to be aware of what it is AND it’s beneficial for us to know what can cause prolapse and what can make it better or even worse. I think it’s important to note what we are experiencing and be aware of what the options are. I talk a lot about knowing your normal so you can know when something is off and this is one of those instances. It is very often that symptoms just don’t go away on their own. In fact, out body is very good at just making things work even when they’re not optimal patterns or habits. Symptoms we may experience include: heaviness or pressure, difficulty peeing or pooping (or standing up and more pee coming out when you’re not ready), incontinence, Low back pain, feeling a bubble or something falling out the vagina, increased discomfort with prolonged standing, or even a funny sensation/pain with sex where it feels as if something is being pressed on deep in the belly. Some of the risk factors to developing prolapse include: *childbirth or vaginal delivery (this could include C-sections where mamas have labored but not delivered vaginally), *higher BMI, *weakness to the pelvic floor, *problems with intra-abdominal pressure like consistent constipation, COPD, chronic cough/allergies *poor posture with intra-abdominal pressure downward (think little old lady bent forward all the time), *perineal tearing/lacerations with delivery or use of assistive devices to pull baby out, *consistent straining to lift heavy items at work or home, *holding breath with activities, *congenital hyper mobility syndrome or diagnosis of Ehlers-Danlos Syndrome, ** see below for self check for hypermobility *menopause (due to lower estrogen levels known to cause pelvic floor weakness or atrophy of the muscles and tissue (this includes hysterectomy!). The best way to check yourself for prolapse is with a mirror in bed. If you are comfortable, you can check your pelvic region at rest and with a bearing down activity like coughing, cleaning your throat or bearing down. If you see something from the front (think behind your pubic bone, it may be your bladder. If you see something from the back, it may be your rectum. If you see something start to descend, ask a professional to check you before you get freaked out!! **Self check for hyper mobility syndrome with this test called the Beighton Scale – Give yourself a point for every item you can do. If you score more than 5/9, you may be hyper mobile and may benefit from more stability work vs stretching to help your body stay stronger and stable. *Pinky bending backwards beyond 90 degrees (1 point for each pinky) *Thumb bending downwards to touch your wrist (1 point for each thumb) *Hyperextension of elbows (straighten elbow and if its past straight give yourself 1 point for each elbow) *Hyperexntension of knees (knees go past straight in standing or locking backwards 1 point for each side) *Bending forward to touching palms to floor (1 point)

What can Priority PT do to help mamas who have organ prolapse?
Kelly: When I took one of my first courses for internal assessment as a Pelvic Floor Physical Therapist several years ago, I was 7 month postpartum and still nursing. I remember lying there and feeling vulnerable (which of course I hate as most of us do!) and found out I had a diagnosis of state 2 rectocele, diastasis recti and painful scarring due to tearing with my daughter years before. I didn’t know I had any of it. How embarrassing to find out at a course and be the subject of learning for others that I had all the things I wanted to help others moms reverse??!! I didn’t feel different aside from knowing my body was weak or just generally de-conditioned from my higher level mentality after delivery and working full time 40+ hours a week standing put more pressure on my already working hard body. I had had 2 vaginal deliveries – one 8 lb baby girl a little more than 2 years before and recently my 5 lb 15 oz son. I remember PUSHING them out. I remember not knowing that I was supposed to let my body do the work and bear down not my pelvic floor muscles or my internal organs. No one told me that bearing down during delivery could cause prolapse. Or what the heck prolapse even was. I thought it was an old lady problem from weak pelvic floor muscles and age. I didn’t know how much I had control over my symptoms until I started learning for myself. I now know that some of the symptoms I had after my daughter were probably prolapse symptoms and I could have been doing more between babies to get stronger, better and more resilient. I now know that the uterus does the work for delivery. The stronger the core muscles or the transverse abdominus, the better the uterus has the ability to contract and push the baby downward. I now know that if I had been able to “breathe” the baby out instead of “PUSHING” the baby out my prolapse may not be as severe….Fast forward 6 years, I am jumping rope up to 1 minute at a time, box jumps, running 2-5 miles should I choose, enjoying sex, and really doing all the things I want to do without hesitation or symptoms (and I know to do my strengthening or unloading exercises on those harder impact days). Why do I tell you this?? Because I want you to know that just because you are diagnosed with a prolapse, it does not mean that you are limited forever. I am determined to give you options to help you make smart decisions around lifting, jumping, taking care of constipation issues, learning how to use your breath as a benefit and not strain, retrain the deep core to help lift up the organs and not push then down further, to teach you how to properly Kegel and WHY they are not the only muscle group we need to improve with prolapse. I am determined to help moms not be scared. I am determine not to let more moms fear running and jumping and trampolining with their kids. I am determined for moms to play actively with their kids and not just watch them have fun for fear of making their symptoms worse. And I am determined to reduce the number of surgeries because moms don’t know that there are other options to help their symptoms. Please also know that the body needs time and consistency to see the changes that so many of us see with training and treatment.
Why are most moms unaware that they have organ prolapse?
Kelly: Though this sounds very scary to hear about – the stats are as high as 50% of women have a type of prolapse. According to one study done in 2014 – out of 9000 women one year (+) after delivery, 89% had uterine prolapse, 90% had cystocele, 70% had rectocele and up to 65% had a grade 2 stage BUT only 20% of these women were symptomatic (that means that up to 80% of these women had no symptoms that made them uncomfortable or aware of a prolapse). Prolapse is something that’s hard to detect unless it’s a higher grade because it’s not a visually obvious problem for most of us. That’s also why it’s important to ask your birth provider to check you after delivery and be made aware of what your status is. Pelvic Floor Physical Therapists can take the information and help you figure out what you are doing on a daily basis and what else you can add to help it from becoming worse. Sometimes it’s not adding on to what you are doing but what you need to avoid doing. Pelvic floor physical therapy should one of the first lines of defense. We can assess the body’s general movement patterns, breathing patterns, bad habits, and strength test specific muscles associated with prolapse. You do not have to jump into surgery and I would highly recommend finding a specialist that can help you determine what your body needs. One of the most common reasons for poor outcomes with surgeries is pelvic floor weakness to begin with.

Do you have a video on this at all?
Kelly: A friend and I were talking about doing mini series…but this is a work in progress! Here is a PDF from the American Urogynecological Society.
Are there any longterm affects of organ prolapse?
Kelly: Long term effects are more of the original but worsening symptoms including difficulty with bowel and bladder emptying, low back pain, discharge thats colored if the internal wall starts to come outside more, pelvic pain, tight muscles in compensation around the pelvis (inner thigh tightness, hip tightness, back tightness). There are often extra supportive structure you can also try called pessaries. These are specifically fitted by a OB/GYN or Uro-gyencologist specifically for your prolapse. Over the counter methods include a trial of tampons, impressa inserts or even tight fitting garments that help to lift up and in the prolapse.
Is there anything else you’d like to share about organ prolapse?
Kelly: Best video out there for hope and an awesome story is Haleys – She has great resources and a story for how she overcame all the scary things we face when we learn we have prolapse. There are often extra supportive structure you can also try called pessaries. These are fitted by a OB/GYN or Uro-gyencologist specifically for your prolapse. Over the counter methods include a trial of tampons, impressa inserts or even tight fitting garments that help to lift up and in the prolapse to determine if something may benefit you. A few quick suggestion for known rectoceles is to use that good ol’ squatty potty. Placing the knees above the hips can help the rectum be in a better position to pass the stool out. Splinting is another option where you insert your finger into the vaginal canal and push gently on the rectum to help the stool pass during a bowel movement.

Thanks so much for sharing such in-depth information about organ prolapse, Kelly! This was super helpful.
If you’re looking for a physical therapist, we highly recommend checking out Priority PT!


